
Introduction to Laser Light Therapy for hair loss
Accidental discovery of Hair Growth
Laser Light Therapy, or Photobiomodulation (PBM) was discovered in 1967 by Endre Mester working at the Semelweiss University in Hungary.1 Mester had obtained an example of the newly invented ruby laser, and commenced a series of experiments designed to answer two questions: (a) can laser irradiation of an experimental tumour transplanted into a mouse or rat produce any cures? (b)does repeated laser irradiation of the skin in a mouse or rat cause skin cancer?
However the ruby laser did not have sufficient power to produce cures in an experimental tumour, and repeated irradiation did not cause any cases of skin cancer.3 Nevertheless these experiments did produce highly interesting and useful results.4 Mester found that incisions that had been made to transplant the tumours healed more rapidly in the laser-treated animals than in controls,5 and moreover the hair grew back faster in the shaved regions of the skin when treated with the ruby laser.6 Mester named this phenomenon “laser biostimulation” and it later became known as “low-level laser therapy” (LLLT).1 Recently an international consensus agreed on the use of the term “photobiomodulation, PBM” to replace LLLT.
Development of Low Level Laser Therapy
Although the early studies mainly used red light (600–700 nm), it was subsequently found that near-infrared (NIR) light (760–1000+ nm) was equally (if not more) effective.9 Light in the low 700 nm regions does not appear to be particularly effective.10,11 This double peak in the action spectrum reflects the absorption spectrum of cytochrome c oxidase (CCO), unit IV in the mitochondrial respiratory chain.12 Together with studies showing the effects of light on isolated mitochondria, these observations led to formation of the most widely-held hypothesis that light stimulates respiration in mitochondria, increasing electron transport, oxygen consumption, and ATP synthesis.13 This stimulation may happen via photodissociation of inhibitory nitric oxide from the heme and copper centres contained within CCO.14
For a number of years the principle uses of laser light therapy (or PBM) were in the areas of wound healing, and reducing pain and inflammation in musculoskeletal disorders.15,16 However starting at the beginning of the 21st century, PBM was actively investigated as a treatment for different forms of hair loss.17–22
Relevance in the treatment of hair loss
Dr. Zakia Rahman on how HairMax is a significant evolution in the treatment of hair loss. from HairMax on Vimeo.
Hair loss or alopecia affects the majority of the population at some time over their lifespan, and those afflicted are increasingly demanding some type of treatment. A healthy head of hair has great social significance for humans. Healthy hair indicates health, youth and vigour. Male pattern baldness is taken to be a sign of age and loss of vigour, which is often concealed or else the entire head is shaved. There is enormous demand for drugs and other treatments that can slow down or reverse hair loss; this has led to the creation of a multibillion-dollar industry.23 In the USA > $3.5 billion is spent every year on treating hair loss.24 It has been stated that “mental disorders such as anxiety, depression, social phobia, posttraumatic stress disorder, and suicidal thoughts are increased among alopecia patients”.25
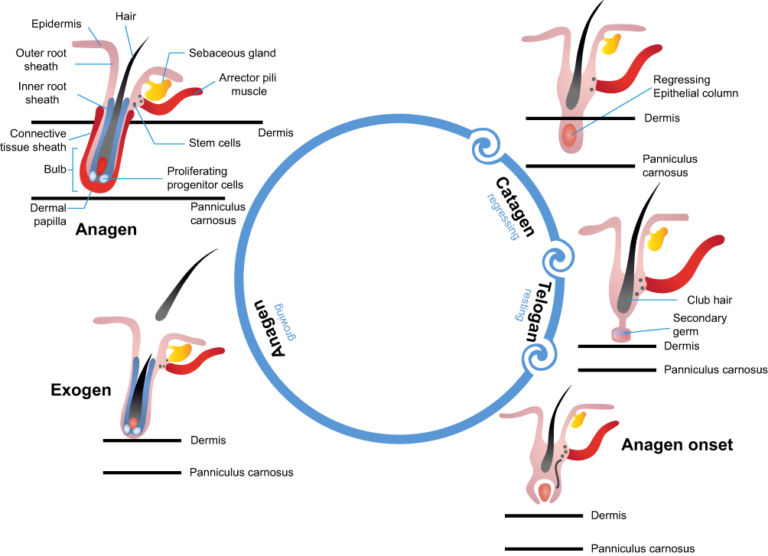
The hair follicle (HF) is a complex mini-organ embedded in the skin and is composed of the papilla, matrix, root sheath and bulge.26 There are between 250,000 and 500,000 HF on the human scalp. Hair grows in cycles during which it moves sequentially from one phase to another (Figure 1). In normal HF the anagen growth phase can last between 2–6 years. This is followed by a short catagen involution-phase, which lasts 1–2 weeks, and then by a telogen resting-phase lasting 5–6 weeks. The old hair is then shed, the anagen phase begins over again, and a new hair is produced. Normally, up to 90% of the HF are in anagen phase, while 10–14% are in telogen and 1–2% in catagen.27
The most important cells in the HF are those in the dermal papilla (DP). These cells produce signals to control sequential cycling of the follicular epithelium.28 It is thought that epithelial stem cells, which reside in the bulge area of the HF, can respond to the signals from the DP. These stem cells give rise to progenitor cells, which then become transiently amplifying cells that migrate downward into the deep dermis. These cells differentiate into matrix cells that actually produce the hair shaft, and the sheath. Several growth factor families are involved in HF cycling, namely fibroblast growth factor, EGF, hepatocyte growth factor, IGF-I, and TGF-β.28 Signal transducer and activator of transcription 3 (stat3) is the most important transcription factor involved in spontaneous HF cycling.29 There is also another stat3-independent pathway involving PKC, which is involved in HF cycling, after plucking for instance.
A series of signaling molecules is involved in each step of primary hair development and differentiation that have been elucidated in studies of embryogenesis.30 Wingless type (Wnt) signalling is crucial for the initiation of HF development.31 Wnt-protein is a ligand that binds to a cell-surface receptor “Frizzled” family member, which then transduces the signal to the intracellular protein “Dishevelled” (Dsh). Dsh causes the accumulation of β-catenin in the cytoplasm (by protecting it from degradation) and its eventual translocation into the nucleus to act as a transcriptional co-activator of transcription factors that belong to the TCF/LEF family.
“Sonic hedgehog” (Shh) signalling plays an important role in both embryonic and adult HF development. Shh binds to and inhibits the extracellular domain “Patched,” allowing the intracellular domain “Smoothened” to accumulate and inhibit the proteolytic cleavage of the Gli family of zinc-finger transcription factors.32
Read: Cure For Baldness – A New Medical Breakthrough Thanks to Sonic Hedgehog
The Three Main Types of Alopecia: Causes and treatment
There are three main types of alopecia; androgenetic alopecia (AGA), alopecia areata (AA) and chemotherapy-induced alopecia (CIA).
Androgenetic alopecia
Androgenetic alopecia (AGA) affects the majority of males as they age, and the distinctive pattern of hair loss is often called “male pattern baldness”.33 The most important predisposing factors are genetic and hormonal, and the balance between two androgen steroids, testosterone and 5α-dihydrotestosterone (DHT). This balance depends on the activity of the enzyme, 5α-reductase in the scalp. Differences in expression of, or polymorphisms in the androgen receptor gene in the HF may also be involved.34 The precise androgen responsive genes in the HF responsible for androgenetic alopecia have yet to be identified. While androgenetic alopecia in women operates by similar molecular mechanisms, the visible pattern of hair loss on the head is different.35
The only widely-employed approved drug therapies for androgenetic alopecia are topical minoxidil (Rogaine®) and oral finasteride (Propecia). In 1988, the FDA approved 2% minoxidil topical solution (Rogaine) for use in treating androgenetic alopecia in men.36 A 2% solution for women became available in 1991, and a 5% solution became available over the counter for use in men in 1997. In 1997, finasteride (Propecia) was approved by the FDA for the treatment of male androgenetic alopecia at a dose of 1 mg/day. This medication is a competitive inhibitor of 5α-reductase that inhibits the conversion of testosterone to DHT, which is involved in miniaturizing the HF in androgenetic alopecia.37
Alopecia Areata – Auto Immune Hair Loss
Alopecia Areata is thought to be an auto-immune disease, in which host T-cells attack the HF. Autoantibodies that bind to epitopes in anagen HF have been found both in affected humans and experimental mouse models.38 Biopsies obtained from affected individuals have shown an inflammatory infiltrate around the anagen HF consisting of activated CD4 and CD8 T lymphocytes.39
In humans Alopecia Areata is sometimes known as spot-baldness with coin shaped areas of hair loss. Alopecia Areata can progress to alopecia totalis (whole scalp) or alopecia universalis (whole body). Individuals with Alopecia Areata are more likely to have another autoimmune disease, and in about 20% of cases there is a family history of AA.40
There is currently no universally proven therapy for Alopecia Areata that induces and sustains remission. Ito41 suggested that since spontaneous remission occurs in 80% of patients within 1 year, and not all patients require intense therapy, that no therapy at all (watchful observation) could be the best option. Topical corticosteroids remain the cornerstone of initial treatment, as indeed they are for many other inflammatory skin disorders.
Chemotherapy-induced Alopecia
Chemotherapy induced Alopecia (or hair loss) is one of the best-known side effects of chemotherapy for cancer. Cancer chemotherapy triggers apoptosis in rapidly dividing cancer cells, but also affects rapidly dividing cells in other tissues (such as the hematopoietic system and the gastrointestinal epithelial lining). Chemotherapy-induced apoptosis depends on the expression of p53, which accumulates in dividing cells after DNA damage, resulting in growth arrest or induction of programmed cell death.42 Many p53-responsive genes are up-regulated, such as Fas, IGF-BP3 and Bax.43 Chemotherapy affects the rapidly proliferating keratinocytes in the bulb region of the anagen HF that are responsible for producing the hair shaft. The HF then enters a dystrophic catagen stage and the hair falls out.
The most often used intervention for Chemotherapy induced Alopecia is scalp-cooling.44 A study reported that use of a scalp-cooling device in women with breast cancer receiving anthracycline and/or taxane based chemotherapy, applied from 30 min before to 90 min after each infusion, preserved hair in 48 out of 95 subjects in the active group and in 0 out of 47 subjects in the sham group.45
Mechanisms of action of Laser Light Therapy in alopecia
How HairMax Laser Light Treatment Works to Regrow Hair from HairMax on Vimeo.
Androgenetic Alopecia and Laser Light Therapy for Hair Regrowth
The results of PBM for androgenetic alopecia suggest that the fraction of all the HF in the anagen phase is increased. This may be due to the ability of PBM to stimulate the mitochondria in the bulge stem cells. Stem cells are quiescent cells that have adapted to survive in their hypoxic niche. One of the most damaging agents to the longevity of cells is oxidative damage to DNA and other biomolecules, caused by the ROS that are an inevitable by-product of aerobic respiration. Therefore stem cells tend to have an overall anaerobic metabolism characterized by low mitochondrial activity and high expression of glycolytic enzymes.46 The low metabolic rate of stem cells accounts for their relative quiescence and increased resistance to stress. Because stem cells must last for such a long time, they have to minimize the number of cell divisions they undergo because each division carries a small risk of DNA damage.
So the hypothesis is that when PBM is delivered to the hypoxic stem cell niche, the rudimentary mitochondria in the stem cells are triggered into action, and mitochondrial biogenesis can take place producing even more mitochondria.47 Increased mitochondrial activity is accompanied by an increasing demand for oxygen, which is not available in the low-oxygen environment of the niche. Therefore the stem cells have to leave their niche in pursuit of the oxygen they need to satisfy their new metabolism involving oxidative phosphorylation. The burst of intracellular ROS that is observed to follow PBM48 may also have a role in triggering the differentiation of stem cells.49 As mentioned above the stem cells, become progenitor cells, transiently amplifying cells and finally matrix cells as the HF enters the anagen phase.
Alopecia areata and Low Level Laser Hair Therapy
The mechanism of action of low level laser light hair therapy has some differences (and some similarities) with that outlined above for AGA. Because alopecia areata is an autoimmune disease, the principle molecular signatures are characteristic of a pro-inflammatory environment in the HF.50 PBM has long been known to have a pronounced anti-inflammatory effect,51 but it is only recently that the possible mechanism for this has become apparent. Cells in the macrophage lineage can assume a diversity of phenotypes, and retain the capability to shift their function to maintain tissue homeostasis. Macrophages can be activated by LPS or IFN‐γ to an M1 phenotype that expresses pro‐inflammatory cytokines and is able to kill microbial cells. On the other hand macrophages can be activated by IL‐4/IL‐13 to an M2 phenotype for phagocytosis of debris, resolution of inflammation and tissue repair. Increasing evidence suggests a role of metabolic reprogramming in the regulation of the innate inflammatory response.52 Studies have demonstrated that the M1 phenotype is often accompanied by a shift from oxidative phosphorylation to aerobic glycolysis for energy production.53 Macrophage activation may be involved in the pathogenesis of autoimmune conditions.54
Since there exists considerable evidence that PBM can activate the mitochondrial metabolism towards oxidative phosphorylation, and away from aerobic glycolysis this is a plausible reason why PBM may change the macrophage phenotype from M1 towards M2.55 The consequences of this shift would be that the highly pro-inflammatory environment that encourages T-cell attack on the HF, would be switched to a less inflammatory environment.
Chemotherapy-induced alopecia
The mechanism of PBM is likely to operate via a different set of signalling pathways. It has long been known that PBM is able to protect cells at risk of dying. Many in vitro models have been utilized to show that PBM can inhibit apoptosis in different cells triggered by a number of different toxic substances. This effect occurs due to the up-regulation of anti-apoptotic proteins, possible in the mitochondria.56 Another group of chromophores was identified in the HF, namely opsins.57 Opsins are blue-light responsive signalling molecules, that were responsible for reducing apoptosis and prolonging the anagen phase in ex vivo HF that were treated with 3.2 J/cm2 of 453 nm LED light.
Laser light therapy for Alopecia
Types of Therapeutic Laser Hair Devices and Parameters
Most of the marketed devices have been based on low power (5 mW) red laser diodes, while some contain LEDs in addition to lasers. The red wavelengths have usually been between 630 nm and 660 nm.
These devices can be divided into four broad types,
- hand held combs or brushes
- head bands
- caps or helmets
- stationary hoods.
The total number of laser diodes incorporated into each of the delivery devices determines the total power administered to the head, and hence the time required to deliver the desired dose to the affected regions of the scalp. Dosimetry is usually measured as an energy density (J/cm2) with a value of 4 J/cm2 frequently quoted. The time of application is usually between 10 and 20 minutes, which can be calculated as the desired fluence of 4 J/cm2 divided by a usual power density of 5 mW/cm2 equals 800 seconds (13.3 minutes). This calculation is arrived at by multiplying the power density of 5 mW/cm2 by the time of 800 seconds to give 4000 mJ/cm2 and dividing the result by 1000 to convert to 4 J/cm2. The treatment repetition for a home use device is usually once per day, but once every two days is also possible. The advantages of a comb or a band device over a cap or a hood, are that the teeth of the laser comb part the hair to allow the light to penetrate better down to the HF.
While all the available evidence suggests that NIR light (800–900 nm) or LED as opposed to laser light would perform as well as red laser light, so far these wavelengths have not been much tested, although in one case a combination of 655 nm and 808 nm was used.58 A recent study looked at different wavelengths of LED (415 nm, 525 nm, 660 nm, 830 nm) on the stimulation of human dermal papilla cells and the elongation of ex vivo HF.59 All four wavelengths showed positive effects, but overall 660 nm was the most efficient. There was significantly increased expression of mRNAs for members of the Wnt signalling pathway that are responsible for cell proliferation, migration and organization (β-catenin, Axin2, Wnt3a, Wnt5a and Wnt10b). LED irradiation significantly increased the expression of β-catenin and cyclin D, and the phosphorylation of MAPK and extracellular signal-regulated kinase (ERK) as determined by Western blot. These genes are also responsible for cell proliferation and migration.
Animal studies and Laser Hair Therapy
Mester’s original study6 involved delivering 1 J of pulsed light from a ruby laser at 694-nm (1 millisecond pulse duration) with a 1 cm2 spot to the depilated abdominal area of black C57BL/6 and white Balb/c mice every week for up to 11 weeks. Before each successive treatment the skin was again depilated. Increased hair growth in the irradiated spot was observed in all black animals between the 5th and 7th treatment. This reaction continued up to the 9th treatment. In white mice no effect on hair growth was detected up to the 8th irradiation, but thereafter hair growth was stimulated to a lesser extent compared to black mice.
Wikramanayake et al reported that PBM could have beneficial effects in a mouse model of AA.60 The model involves topical application of focal heat to the skin of C3H/HeJ mice leading to hair loss accompanied by intra-follicular and peri-follicular mononuclear cell infiltrates in the anagen HF.61 Affected regions of mouse skin were treated with a 655 nm laser for 20 s daily, three times per week for 6 weeks. Hair regrowth was first observed in the PBM group after 2 weeks of laser treatment and at 6 weeks there was complete hair regrowth in all six mice. In the sham group there was no regrowth of hair at 6 weeks.
The same group (Wikramanayake et al) also reported the use of PBM to treat CIA in a rat model.62 The chemotherapy agents, cyclophosphamide, etoposide, or a combination of cyclophosphamide and doxorubicin were administered to two-week old rats to induce whole body alopecia 7–10 days later. The rats received PBM (655 nm laser) for 1 min once daily for 10 days. Rats receiving laser treatment regrew hair 5 days earlier than rats receiving chemotherapy alone or sham laser treatment. The authors checked that the PBM treatment did not protect subcutaneously injected cancer cells from the effects of the chemotherapy.
Clinical studies in Laser Hair Therapy
Most clinical trials so far reported have been carried out for androgenetic alopecia in either men or women. One of the first reports used the HairMax Laser Comb (655 nm laser) in a double-blind, sham-controlled, multicentre, 26-week trial with 110 randomized males with Norwood-Hamilton classes IIa-V AGA. Patients were treated for 15 min three times per week for 26 weeks.63 Subjects receiving active PBM showed a mean increase in hair density (+17.3±11.9 hairs/cm2) while those receiving sham had a decrease (−8.9+11.7), p<0.0001. Kim et al used a helmet type device containing 630 nm and 660 nm LEDs and 650 nm laser diodes.64 They recruited 40 subjects comprising 26 men (Norwood-Hamilton III–VII) and 14 women (Ludwig I–III) with AGA. Subjects were treated for 15 min once every day for 24 weeks. Subjects receiving active treatment showed a mean increase in hair density of +17.2+12.1 while subjects receiving sham showed a decrease of −2.1+18.3, p=0.003. There was also a significant increase in hair thickness in active treated subjects. Lanzafame et al published a pair of papers describing trials of a helmet device consisting of 655 nm LEDs and 655 nm lasers on 44 males65 and 47 females.66 Patients were treated for 25 min every two days for 16 weeks. The men showed a 62.5% increase in hair counts in the active group vs a 37% increase in sham group (p=0.003).65 The women showed a 48% increase in hair count in the active group vs a 11% increase in the sham group (p<0.001).66
Other groups have reported significant improvements in hair regrowth in both men (128 subjects) and women (141 subjects) using a HairMax Laser Comb,67 and in 44 females using a laser cap device.68 Barikbin et al compared the effects of a 655 nm laser cap and a laser scanner combining 655 nm and 808 nm in 90 subjects.58 Both devices significantly improved hair counts but the 655/808 nm combination was slightly better. In all cases, the incidence of side effects was rare (<10%), tolerable and transient.69 Dry skin, irritation, pruritis and mild headache were the most often reported side effects.
Esmet et al compared topical minoxidil 5% with PBM using an iGrow helmet and the combination of both therapies in 45 women with AGA.70 Topical minoxidil was applied twice daily, and PBM was used for 25 min 3 days a week for the 16-week study duration. All groups were effective, but the combination group showed a benefit earlier (at 2 months) compared to the monotherapies.
There have been few clinical trials of PBM for alopecia areata. One conducted by Yamazaki et used a “SuperLizer” device that emits linear polarized light over a wavelength range of 600–1600 nm.71 Fifteen patients with patchy hair loss, were treated on some areas for 3 min once every 1 or 2 weeks for up to 5 months, while other areas acted as controls. 46.7% of the treated areas showed hair regrowth, 1.6 months earlier than the non-irradiated areas (p=0.003).
I cannot trace any publication of a clinical trial for CIA although some studies have been proposed.
Who should use Laser Hair therapy?
Patient selection should take account of the following points. Both men and women with AGA respond very well to PBM. However because men generally have higher levels of DHT (and testosterone) compared to women, the continuing pressure exerted by hormonal influences is more pronounced in men. Therefore the PBM is constantly fighting against the influence of DHT, and may have to be periodically used throughout the entire lifetime. This consideration may explain why some trials of PBM have shown somewhat better results in women compared to men. Due to the rather gradual benefits of PBM for alopecia, it makes a lot of sense to commence treatment sooner rather than later. Ideally treatment should commence at the earliest stage of self-perceived thinning hair. In shiny bald scalps as are seen in some men, the HF are gone forever, and no amount of PBM will bring the follicles back from the dead. The question is sometimes raised about different pigmentation levels of hair and skin and whether this affects the benefits of PBM. Undoubtedly hair is a barrier to light penetration, and thick dark hair is a considerable barrier. However since the light is most required in areas of hair loss, this may not be a big problem in reality. As regards pigment levels in skin, it is believed that dark skin (Fitzpatrick skin types IV–VI) require higher doses of light (longer exposure to a PBM device) compared to light skin (Fitzpatrick skin types I–III), although this hypothesis has not yet been fully tested in a clinical trial. The study showing an increased benefit of combining topical minoxidil with PBM70 suggests further combination studies should be explored. The use of PBM in combination with hair transplantation surgery has been discussed, but as yet there are no published studies. PBM is proposed to be able to encourage the integration of the transplanted hair grafts and also to hasten the healing of the donor sites. Moreover some investigators are considering the combination of PBM with platelet rich plasma (PRP). PRP is a growing technology for treatment of AGA involving the injection into the scalp of autologous PRP at monthly intervals for 3 months.72 In some cases the PRP can be activated before injection using calcium chloride,73 and PBM has been proposed as an alternative method to activate PRP.
The use of PBM in cases of AA has not been investigated to anything like the same level as PBM for AGA. This is probably because AA is fairly rare, while AGA affects the majority of the population.
The use of PBM should be tested in patients undergoing chemotherapy for cancer (probably women with breast cancer). It is suggested that consideration should be given to commencing PBM a few days before initiation of chemotherapy as well as during the infusion itself, to give the HF a chance to upregulate anti-apoptotic proteins.
Perspectives
The use of PBM for hair regrowth still remains contentious. This is despite an ever-growing number of clinical trials reporting positive results, mainly in AGA. Nevertheless some studies have used relatively small sample sizes, and there may be a perceived risk of bias in other studies. Perhaps another reason for this lack of universal acceptance, is the fact that PBM requires fairly prolonged application over a period of months to achieve the optimal effects. This was probably unrealistic when PBM was generally applied in clinics or salons. Some individuals probably gave up when they did not see rapid results, or else expected PBM to work in relatively advanced cases of AGA. Moreover some companies have marketed PBM in an unrealistic fashion, encouraging over-optimistic expectations. Now that home use PBM devices are becoming widely available, and also the fact that LED devices are becoming more common, perhaps we can expect that the public acceptance will increase. Well-controlled clinical trials of PBM in patients with AA and CIA are urgently required.
Disclosure
Michael R Hamblin was supported by US NIH Grants R01AI050875 and R21AI121700. Michael R Hamblin is on the following scientific advisory boards: Transdermal Cap Inc, Cleveland, OH; BeWell Global Inc, Wan Chai, Hong Kong; Hologenix Inc, Santa Monica, CA; LumiThera Inc, Poulsbo, WA; Vielight, Toronto, Canada; Bright Photomedicine, Sao Paulo, Brazil; Quantum Dynamics LLC, Cambridge, MA; Global Photon Inc, Bee Cave, TX; Medical Coherence, Boston MA; NeuroThera, Newark DE; JOOVV Inc, Minneapolis-St. Paul MN; AIRx Medical, Pleasanton CA; FIR Industries, Inc. Ramsey, NJ; UVLRx Therapeutics, Oldsmar, FL; Ultralux UV Inc, Lansing MI; Illumiheal and PetThera, Shoreline, WA; MB Lasertherapy, Houston, TX; ARRC LED, San Clemente, CA; Varuna Biomedical Corp. Incline Village, NV; Niraxx Light Therapeutics, Inc, Boston, MA. Dr Hamblin has been a consultant for Lexington Int, Boca Raton, FL; USHIO Corp, Japan; Merck KGaA, Darmstadt, Germany; Philips Electronics Nederland B.V.; Johnson & Johnson Inc, Philadelphia, PA; Sanofi-Aventis Deutschland GmbH, Frankfurt am Main, Germany. Dr Hamblin is a stockholder in Global Photon Inc, Bee Cave, TX; Mitonix, Newark, DE. The author reports no other conflicts of interest in this work.
References
Original article – https://www.dovepress.com/photobiomodulation-for-the-management-of-alopecia-mechanisms-of-action-peer-reviewed-fulltext-article-CCID#CIT0025
- Mester A, Mester A. The history of photobiomodulation: endre mester (1903-1984). Photomed Laser Surg. 2017;35:393–394. doi:10.1089/pho.2017.4332
- McGuff PE, Deterling RA Jr., Gottlieb LS. Tumoricidal effect of laser energy on experimental and human malignant tumors. N Engl J Med. 1965;273:490–492. doi:10.1056/NEJM196508262730906
- Mester E, Szende B, Tota JG. [Effect of low intensity laser radiation, repeatedly administered over a long period, on the skin and inner organs of mice]. Radiobiol Radiother (Berl). 1969;10:371–377.
- Mester E, Jaszsagi-Nagy E. Biological effects of laser radiation. Radiobiol Radiother (Berl). 1971;12:377–385.
- Mester E, Szende B, Spiry T, Scher A. Stimulation of wound healing by laser rays. Acta Chir Acad Sci Hung. 1972;13:315–324.
- Mester E, Szende B, Gartner P. [The effect of laser beams on the growth of hair in mice]. Radiobiol Radiother (Berl). 1968;9:621–626.
- Anders JJ, Lanzafame RJ, Arany PR. Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg. 2015;33:183–184. doi:10.1089/pho.2015.9848
- Heiskanen V, Hamblin MR. Photobiomodulation: lasers vs. Light Emitting Diodes? Photochem Photobiol Sci. 2018;17:1003–1017. doi:10.1039/c8pp90049c
- Lubart R, Wollman Y, Friedmann H, Rochkind S, Laulicht I. Effects of visible and near-infrared lasers on cell cultures. J Photochem Photobiol B. 1992;12:305–310.
- Gupta A, Dai T, Hamblin MR. Effect of red and near-infrared wavelengths on low-level laser (light) therapy-induced healing of partial-thickness dermal abrasion in mice. Lasers Med Sci. 2013;29(1):257–265.
- Wu Q, Xuan W, Ando T, et al. Low-level laser therapy for closed-head traumatic brain injury in mice: effect of different wavelengths. Lasers Surg Med. 2012;44:218–226. doi:10.1002/lsm.22003
- Wong-Riley MT, Liang HL, Eells JT, et al. Photobiomodulation directly benefits primary neurons functionally inactivated by toxins: role of cytochrome c oxidase. J Biol Chem. 2005;280:4761–4771. doi:10.1074/jbc.M409650200
- Karu TI. Multiple roles of cytochrome c oxidase in mammalian cells under action of red and IR-A radiation. IUBMB Life. 2010;62:607–610. doi:10.1002/iub.359
- Lane N. Cell biology: power games. Nature. 2006;443:901–903. doi:10.1038/443901a
- Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40:516–533. doi:10.1007/s10439-011-0454-7
- Hamblin MR, Ferraresi C, Huang YY, de Freitas LF, Carroll JD. Low-Level Light Therapy: Photobiomodulation. Bellingham (WA): SPIE Press; 2018.
- Avci P, Gupta GK, Clark J, Wikonkal N, Hamblin MR. Low-level laser (light) therapy (LLLT) for treatment of hair loss. Lasers Surg Med. 2014;46:144–151. doi:10.1002/lsm.22170
- Darwin E, Arora H, Hirt PA, Wikramanayake TC, Jimenez JJ. A review of monochromatic light devices for the treatment of alopecia areata. Lasers Med Sci. 2018;33:435–444. doi:10.1007/s10103-017-2412-6
- Darwin E, Heyes A, Hirt PA, Wikramanayake TC, Jimenez JJ. Low-level laser therapy for the treatment of androgenic alopecia: a review. Lasers Med Sci. 2018;33:425–434. doi:10.1007/s10103-017-2385-5
- Delaney SW, Zhang P. Systematic review of low-level laser therapy for adult androgenic alopecia. J Cosmet Laser Ther. 2018;20:229–236. doi:10.1080/14764172.2017.1400170
- Gupta AK, Daigle D. The use of low-level light therapy in the treatment of androgenetic alopecia and female pattern hair loss. J Dermatolog Treat. 2014;25:162–163. doi:10.3109/09546634.2013.832134
- Gupta AK, Lyons DC, Abramovits W. Low-level laser/light therapy for androgenetic alopecia. Skinmed. 2014;12:145–147.
- Semalty M, Semalty A, Joshi GP, Rawat MS. Hair growth and rejuvenation: an overview. J Dermatolog Treat. 2011;22:123–132. doi:10.3109/09546630903578574
- Statista.com; 2017. Available from: https://www.statista.com/statistics/489025/value-of-the-global-hair-loss-treatment-market/. Accessed August 16, 2019.
- Gokalp H. Psychosocial aspects of hair loss. In: Kutlubay Z, Serdaroglu S, editors. Hair and Scalp Disorders. London, UK: IntechOpen; 2016.
- Paus R, Muller-Rover S, Van Der Veen C, et al. A comprehensive guide for the recognition and classification of distinct stages of hair follicle morphogenesis. J Invest Dermatol. 1999;113:523–532. doi:10.1046/j.1523-1747.1999.00740.x
- Burg D, Yamamoto M, Namekata M, Haklani J, Koike K, Halasz M. Promotion of anagen, increased hair density and reduction of hair fall in a clinical setting following identification of FGF5-inhibiting compounds via a novel 2-stage process. Clin Cosmet Investig Dermatol. 2017;10:71–85. doi:10.2147/CCID.S123401
- Peus D, Pittelkow MR. Growth factors in hair organ development and the hair growth cycle. Dermatol Clin. 1996;14:559–572.
- Sano S, Kira M, Takagi S, Yoshikawa K, Takeda J, Itami S. Two distinct signaling pathways in hair cycle induction: Stat3-dependent and -independent pathways. Proc Natl Acad Sci U S A. 2000;97:13824–13829. doi:10.1073/pnas.240303097
- Rishikaysh P, Dev K, Diaz D, Qureshi WM, Filip S, Mokry J. Signaling involved in hair follicle morphogenesis and development. Int J Mol Sci. 2014;15:1647–1670. doi:10.3390/ijms15011647
- Andl T, Reddy ST, Gaddapara T, Millar SE. WNT signals are required for the initiation of hair follicle development. Dev Cell. 2002;2:643–653.
- Harris PJ, Takebe N, Ivy SP. Molecular conversations and the development of the hair follicle and basal cell carcinoma. Cancer Prev Res (Phila). 2010;3:1217–1221. doi:10.1158/1940-6207.CAPR-10-0210
- Ellis JA, Sinclair R, Harrap SB. Androgenetic alopecia: pathogenesis and potential for therapy. Expert Rev Mol Med. 2002;4:1–11. doi:10.1017/S1462399402005112
- Ellis JA, Stebbing M, Harrap SB. Polymorphism of the androgen receptor gene is associated with male pattern baldness. J Invest Dermatol. 2001;116:452–455. doi:10.1046/j.1523-1747.2001.01261.x
- Herskovitz I, Tosti A. Female pattern hair loss. Int J Endocrinol Metab. 2013;11:e9860. doi:10.5812/ijem
- Rossi A, Cantisani C, Melis L, Iorio A, Scali E, Calvieri S. Minoxidil use in dermatology, side effects and recent patents. Recent Pat Inflamm Allergy Drug Discov. 2012;6:130–136.
- Rittmaster RS. Finasteride. N Engl J Med. 1994;330:120–125. doi:10.1056/NEJM199401133300208
- Tobin DJ. Characterization of hair follicle antigens targeted by the anti-hair follicle immune response. J Investig Dermatol Symp Proc. 2003;8:176–181. doi:10.1046/j.1087-0024.2003.00805.x
- Gilhar A, Paus R, Kalish RS. Lymphocytes, neuropeptides, and genes involved in alopecia areata. J Clin Invest. 2007;117:2019–2027. doi:10.1172/JCI31942
- Spano F, Donovan JC. Alopecia areata: part 1: pathogenesis, diagnosis, and prognosis. Can Fam Physician. 2015;61:751–755.
- Ito T. Advances in the management of alopecia areata. J Dermatol. 2012;39:11–17. doi:10.1111/j.1346-8138.2011.01476.x
- Borges HL, Linden R, Wang JY. DNA damage-induced cell death: lessons from the central nervous system. Cell Res. 2008;18:17–26. doi:10.1038/cr.2007.110
- Botchkarev VA, Komarova EA, Siebenhaar F, et al. p53 is essential for chemotherapy-induced hair loss. Cancer Res. 2000;60:5002–5006.
- Ross M, Fischer-Cartlidge E. Scalp cooling: a literature review of efficacy, safety, and tolerability for chemotherapy-induced alopecia. Clin J Oncol Nurs. 2017;21:226–233. doi:10.1188/17.CJON.226-233
- Nangia J, Wang T, Osborne C, et al. Effect of a scalp cooling device on alopecia in women undergoing chemotherapy for breast cancer: the SCALP randomized clinical trial. JAMA. 2017;317:596–605. doi:10.1001/jama.2016.20939
- Simsek T, Kocabas F, Zheng J, et al. The distinct metabolic profile of hematopoietic stem cells reflects their location in a hypoxic niche. Cell Stem Cell. 2010;7:380–390. doi:10.1016/j.stem.2010.07.011
- Tatmatsu-Rocha JC, Tim CR, Avo L, et al. Mitochondrial dynamics (fission and fusion) and collagen production in a rat model of diabetic wound healing treated by photobiomodulation: comparison of 904nm laser and 850nm light-emitting diode (LED). J Photochem Photobiol B. 2018;187:41–47. doi:10.1016/j.jphotobiol.2018.07.032
- Chen AC, Arany PR, Huang YY, et al. Low-level laser therapy activates NF-kB via generation of reactive oxygen species in mouse embryonic fibroblasts. PLoS One. 2011;6:e22453. doi:10.1371/journal.pone.0022453
- Owusu-Ansah E, Banerjee U. Reactive oxygen species prime Drosophila haematopoietic progenitors for differentiation. Nature. 2009;461:537–541. doi:10.1038/nature08313
- Jabbari A, Cerise JE, Chen JC, et al. Molecular signatures define alopecia areata subtypes and transcriptional biomarkers. EBioMedicine. 2016;7:240–247. doi:10.1016/j.ebiom.2016.03.036
- Hamblin MR. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys. 2017;4:337–361. doi:10.3934/biophy.2017.3.337
- Orihuela R, McPherson CA, Harry GJ. Microglial M1/M2 polarization and metabolic states. Br J Pharmacol. 2016;173:649–665. doi:10.1111/bph.13139
- Haschemi A, Kosma P, Gille L, et al. The sedoheptulose kinase CARKL directs macrophage polarization through control of glucose metabolism. Cell Metab. 2012;15:813–826. doi:10.1016/j.cmet.2012.04.023
- Ushio A, Arakaki R, Yamada A, et al. Crucial roles of macrophages in the pathogenesis of autoimmune disease. World J Immunol. 2017;7:1–8. doi:10.5411/wji.v7.i1.1
- Fernandes KP, Souza NH, Mesquita-Ferrari RA, et al. Photobiomodulation with 660-nm and 780-nm laser on activated J774 macrophage-like cells: effect on M1 inflammatory markers. J Photochem Photobiol B. 2015;153:344–351. doi:10.1016/j.jphotobiol.2015.10.015
- Yin K, Zhu R, Wang S, Zhao RC. Low-level laser effect on proliferation, migration, and antiapoptosis of mesenchymal stem cells. Stem Cells Dev. 2017;26:762–775. doi:10.1089/scd.2016.0332
- Buscone S, Mardaryev AN, Raafs B, et al. A new path in defining light parameters for hair growth: discovery and modulation of photoreceptors in human hair follicle. Lasers Surg Med. 2017;49:705–718. doi:10.1002/lsm.22673
- Barikbin B, Khodamrdi Z, Kholoosi L, et al. Comparison of the effects of 665 nm low level diode laser hat versus and a combination of 665 nm and 808nm low level diode laser scanner of hair growth in androgenic alopecia. J Cosmet Laser Ther. 2017. doi:10.1080/14764172.2017.1326609
- Joo HJ, Jeong KH, Kim JE, Kang H. Various wavelengths of light-emitting diode light regulate the proliferation of human dermal papilla cells and hair follicles via Wnt/beta-Catenin and the extracellular signal-regulated kinase pathways. Ann Dermatol. 2017;29:747–754. doi:10.5021/ad.2017.29.6.747
- Wikramanayake TC, Rodriguez R, Choudhary S, et al. Effects of the Lexington LaserComb on hair regrowth in the C3H/HeJ mouse model of alopecia areata. Lasers Med Sci. 2012;27:431–436. doi:10.1007/s10103-011-0953-7
- Wikramanayake TC, Alvarez-Connelly E, Simon J, et al. Heat treatment increases the incidence of alopecia areata in the C3H/HeJ mouse model. Cell Stress Chaperones. 2010;15:985–991. doi:10.1007/s12192-010-0209-7
- Wikramanayake TC, Villasante AC, Mauro LM, et al. Low-level laser treatment accelerated hair regrowth in a rat model of chemotherapy-induced alopecia (CIA). Lasers Med Sci. 2013;28:701–706. doi:10.1007/s10103-012-1139-7
- Leavitt M, Charles G, Heyman E, Michaels D. HairMax LaserComb laser phototherapy device in the treatment of male androgenetic alopecia: a randomized, double-blind, sham device-controlled, multicentre trial. Clin Drug Investig. 2009;29:283–292. doi:10.2165/00044011-200929050-00001
- Kim H, Choi JW, Kim JY, Shin JW, Lee SJ, Huh CH. Low-level light therapy for androgenetic alopecia: a 24-week, randomized, double-blind, sham device-controlled multicenter trial. Dermatol Surg. 2013;39:1177–1183. doi:10.1111/dsu.12200
- Lanzafame RJ, Blanche RR, Bodian AB, Chiacchierini RP, Fernandez-Obregon A, Kazmirek ER. The growth of human scalp hair mediated by visible red light laser and LED sources in males. Lasers Surg Med. 2013;45:487–495. doi:10.1002/lsm.22173
- Lanzafame RJ, Blanche RR, Chiacchierini RP, Kazmirek ER, Sklar JA. The growth of human scalp hair in females using visible red light laser and LED sources. Lasers Surg Med. 2014;46:601–607. doi:10.1002/lsm.22277
- Jimenez JJ, Wikramanayake TC, Bergfeld W, et al. Efficacy and safety of a low-level laser device in the treatment of male and female pattern hair loss: a multicenter, randomized, sham device-controlled, double-blind study. Am J Clin Dermatol. 2014;15:115–127. doi:10.1007/s40257-013-0060-6
- Friedman S, Schnoor P. Novel approach to treating androgenetic alopecia in females with photobiomodulation (low-level laser therapy). Dermatol Surg. 2017;43:856–867. doi:10.1097/DSS.0000000000001114
- Liu KH, Liu D, Chen YT, Chin SY. Comparative effectiveness of low-level laser therapy for adult androgenic alopecia: a system review and meta-analysis of randomized controlled trials. Lasers Med Sci. 2019;34:1063–1069. doi:10.1007/s10103-019-02723-6
- Esmat SM, Hegazy RA, Gawdat HI, et al. Low level light-minoxidil 5% combination versus either therapeutic modality alone in management of female patterned hair loss: a randomized controlled study. Lasers Surg Med. 2017;49:835–843. doi:10.1002/lsm.22684
- Yamazaki M, Miura Y, Tsuboi R, Ogawa H. Linear polarized infrared irradiation using Super Lizer is an effective treatment for multiple-type alopecia areata. Int J Dermatol. 2003;42:738–740. doi:10.1046/j.1365-4362.2003.01968.x
- Ferneini EM, Beauvais D, Castiglione C, Ferneini MV. Platelet-rich plasma in androgenic alopecia: indications, technique, and potential benefits. J Oral Maxillofac Surg. 2017;75:788–795. doi:10.1016/j.joms.2016.10.040
- Ince B, Yildirim MEC, Dadaci M, Avunduk MC, Savaci N. Comparison of the efficacy of homologous and autologous Platelet-Rich Plasma (PRP) for treating androgenic alopecia. Aesthetic Plast Surg. 2018;42:297–303. doi:10.1007/s00266-017-1004-y



